AI-generated summary
The fusion of neurotechnology, artificial intelligence (AI), and immersive environments like augmented reality (AR) and virtual reality (VR) is revolutionizing 21st-century medicine. Once experimental, AR and VR have become essential tools for diagnosis, surgical training, and therapy worldwide. Professor Didier Stricker of the German Research Center for Artificial Intelligence highlights applications such as musculoskeletal rehabilitation, surgical guidance with real-time data overlays, and intraoperative navigation that enhance precision, safety, and remote collaboration. These technologies enable risk-free, realistic simulation environments to train medical professionals, improving their skills and confidence. Leading European centers are adopting immersive 3D visualizations for anatomy education and clinical training.
Beyond surgery, immersive tech transforms rehabilitation by providing personalized motor and cognitive therapy through adaptable virtual scenarios. Systems incorporate AI to tailor treatments to individual patients, aiding recovery from stroke and motor injuries while addressing cognitive functions like memory and attention. VR also reduces pain perception and anxiety during procedures by immersing patients in calming virtual environments. Moreover, AI-powered AR supports assisted diagnosis and remote therapies, enhancing healthcare accessibility and equity by enabling hospital-level care at home. Despite challenges in ethics, data privacy, certification, and costs, these technologies promise a future where medicine is more precise, personalized, and humane. The goal is not to replace healthcare professionals but to augment human capacity and strengthen the patient-caregiver relationship through immersive, interactive experiences.
The fusion between Neurotechnology, artificial intelligence and immersive environments are transforming medicine. In particular, augmented reality (AR) and virtual reality (VR) —and their evolution into mixed reality—are no longer mere experimental tools: they have become tools for diagnosis, training, and therapy in hospitals around the world. Didier Stricker, professor at the Technical University of Kaiserslautern […]
The fusion between Neurotechnology, artificial intelligence and immersive environments are transforming medicine. In particular, augmented reality (AR) and virtual reality (VR) —and their evolution into mixed reality—are no longer mere experimental tools: they have become tools for diagnosis, training, and therapy in hospitals around the world. Didier Stricker, professor at the Technical University of Kaiserslautern and scientific director of the Department of Augmented Vision at the German Research Center for Artificial Intelligence (DFKI), has been exploring this boundary between the physical and the digital for more than two decades. With their help we will try to outline the present and the future that these technologies are drawing.
From simulation to operating room
The Medicine of the 21st century is experiencing a silent revolution. With headsets such as Microsoft’s HoloLens or platforms developed by pioneering centers around the world, students and surgeons train in three-dimensional environments where error no longer costs lives. VR allows complex operations to be performed or emergencies to be managed without risk, while AR superimposes vital data and radiological images directly on the patient’s body.
“The most promising applications of cognitive augmented reality in health,” Professor Stricker explains to the Bankinter Innovation Foundation, “range from musculoskeletal rehabilitation and motor learning – with real-time kinematic feedback and accompaniment in adherence to treatment – to surgical guidance and intraoperative navigation, with contextual layers that show tool trajectories, no-go zones, hands-free checklists and telementoring.” This ability to see through the body adds a new dimension to clinical work: precision, safety, and remote cooperation.
The benefits are beginning to be measured: studies show that professionals trained with VR improve their accuracy and confidence in critical situations, from emergency simulations to laparoscopic surgery. In Spain, centres such as the Hospital Clínic de Barcelona or the University of Zaragoza are already using immersive simulation environments for medical training, while European universities such as Padua or Marseille apply these technologies to the teaching of anatomy, replacing physical models with interactive 3D visualisations that the student can explore from any angle.
Rehabilitate the body… and the mind
Beyond the operating room, immersive technologies are also reconfiguring rehabilitation. In patients with stroke or motor injuries, virtual environments allow repetitive exercises to be performed in realistic and adaptive scenarios, where each movement generates immediate feedback . Stricker sums up this transformation this way: “Thanks to the combination of AI and augmented vision, we can offer personalized cognitive and motor training.” According to the expert, these systems take into account the patient’s limitations and adapt treatments accordingly. But cognitive augmented reality isn’t limited to the physical aspect.
It is also used in cognitive therapy and neurorehabilitation, training attention, memory and visuospatial perception through dynamics of adaptive difficulty or controlled XR environments that allow progressive exposure to complex stimuli. Constant interaction maintains motivation and reinforces adherence to treatments, a crucial aspect in a context of shortage of health personnel and an aging population.
In Switzerland, the start-up MindMaze , with which the Kaiserslautern team collaborates, uses VR headsets and neural sensors to help stroke victims regain control of their limbs. Other European projects, such as ShareSpace, validate remote rehabilitation environments with avatars that reproduce the therapist and accompany the patient at home, expanding the scope of therapy and reducing travel.
Immersion not only accelerates physical recovery: it also influences pain perception and emotional well-being. Clinical studies—such as the one on St George’s Hospital in London or the Research by Hoffman and Li on immersive analgesia—shows that patients undergoing painful procedures report less anxiety and up to 50% less pain sensation when using VR headsets that transport them to natural landscapes or relaxing environments. “VR/AR has a strong cognitive dimension,” Stricker said, “and can be used both to improve pain management and to increase patient engagement through more engaging environments and tools.”
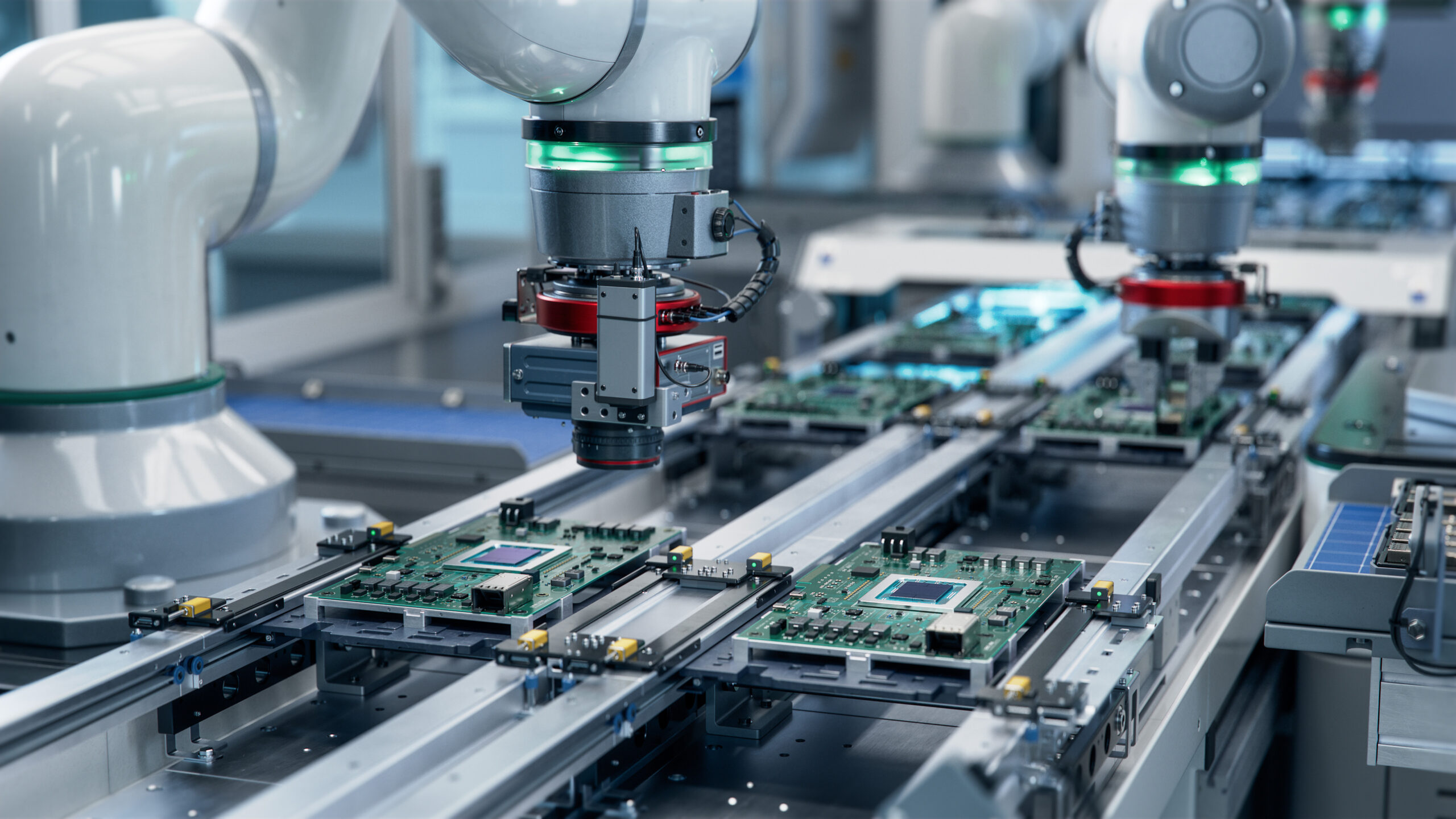
Smart diagnostics and remote therapies
The convergence between augmented vision and artificial intelligence opens up another horizon: assisted diagnosis. “A cognitive augmented reality system can offer a second opinion to the doctor or physiotherapist. It saves time and increases safety,” says Stricker. In this area, his group has developed tools for automatic analysis of ultrasound images through the start-up ANNA-Ctrus, capable of detecting anomalies with computer vision algorithms.
The added value of XR (extended reality) also lies in its ability to democratize healthcare. In fact, thanks to connectivity and wearable sensors, patients can receive accurate feedback from home, maintaining the quality of a hospital follow-up. “I’m especially interested in remote cooperation,” adds the professor. “The ability for a therapist to guide exercises or monitor progress through immersive environments opens up a new model of health equity.”
The XR thus enhances remote access and fairness: it allows shorter and more frequent sessions, without traveling, offering hospital-level feedback in the home itself. European projects such as VR Health Champions, promoted by the Bruno Kessler Foundation together with eighteen other partners, are working in precisely this direction: to integrate VR and AR solutions into daily clinical practice with common standards and certifications that guarantee their effectiveness and dissemination. Among the participating SMEs are companies such as Meeva, which develops virtual therapies for neurodivergent youth, and LightSpace, specialized in augmented surgery.
Ethics, personalization and the future
The accelerated development of these technologies also poses new dilemmas. AR and VR don’t just collect biometric data: they record gestures, emotions, reaction times. How to guarantee the privacy and autonomy of the patient when the body itself becomes an interface? Stricker puts it clearly: “My biggest ethical concern is to preserve patient autonomy and integrity when using immersive technologies. The patient must remain in the driver’s seat.”
At the same time, the Personalization that artificial intelligence allows redefines the very concept of treatment. XR does not replace the professional, but expands its reach: it offers more information, more control and, above all, more humanity. By actively involving the patient—whether in a physical therapy session or a pre-operative simulation—the experience becomes participatory and empathetic.
The barriers are not minor: medical certifications, hardware costs, stability of systems, staff training. But the technical advances are dizzying. According to Stricker, “the Artificial intelligence is the core enabling technology of extended reality. It is transforming the creation of 3D content, the narrative of scenes, the realism of rendering and the appearance of avatars with more human behaviors, capable of reasoning, responding and acting with a certain autonomy.”
The immersive revolution no longer belongs only to the world of entertainment. The The combination of AI, neurotechnology and augmented vision is building a new medicine, more precise and closer. From connected operating rooms to remote cognitive therapies, each breakthrough reveals the same purpose: to expand human capacity without losing the human bond. The future of augmented and virtual reality is not about replacing us, but about helping us better understand who we are and what we can do.